Breadcrumb
A comprehensive patient-specific prediction model for temporomandibular joint osteoarthritis progression
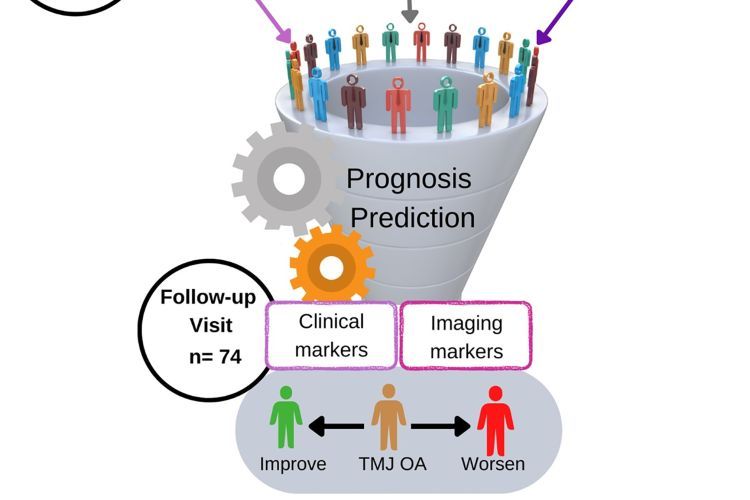
Schematic representation for the steps of the TMJ OA prognosis prediction model’s development. (A) Clinical, imaging, and biological data were collected from the study subjects, at baseline, and utilized to create the OA Prognosis Prediction model.
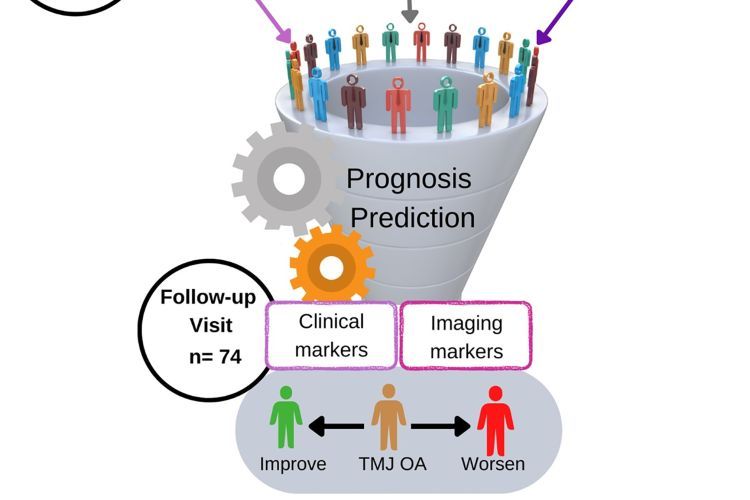
(B) Clinical and imaging data were collected, at follow-up visits, to label the training dataset with the changes of the participants’ health status following 2 to 3 y of conservative management.
What is it?
Temporomandibular joint osteoarthritis (TMJ OA) is a common condition causing jaw pain and difficulty moving the jaw.
What problem does it aim to solve?
The study aimed to improve prediction of how TMJ OA progresses and how patients respond to treatment.
How does it work?
Researchers followed 106 patients, with 74 of them getting checked after 2 to 3 years of non-surgical treatment. This study identified a comprehensive set of clinical, quantitative imaging, and biological biomarkers for precise prediction of TMJ OA disease progression. Researchers developed an open-source tool based on a robust method called Ensemble via Hierarchical Predictions through Nested cross-validation (EHPN), which surpassed the performance of the 48 models tested. The EHPN model achieved an F1 score of 0.82, indicating strong performance and reliability with new, unseen data, and minimizing false positives and negatives.
What are the real-world implications?
The use of the EHPN model may revolutionize the standards of care, providing clinicians with an accurate tool for anticipating the future status of TMJ OA patients, thereby enhancing their decision-making process.
What are the next steps?
Further refinement of the model.
Source
“A comprehensive patient-specific prediction model for temporomandibular joint osteoarthritis progression”, Proceedings of the National Academy of Sciences USA 2024 Vol. 121 No. 8
Authors
Najla Al Turkestani
Department of Restorative Dentistry, Faculty of Dentistry, King Abdulaziz University, Jeddah 21589, Saudi Arabia
Department of Orthodontics and Pediatric Dentistry, School of Dentistry, University of Michigan, Ann Arbor, MI 48109
Tengfei Li
Department of Psychiatry, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
Jonas Bianchi
Department of Orthodontics, University of the Pacific, Arthur A. Dugoni School of Dentistry, San Francisco, CA 94103
Marcela Gurgel
Department of Orthodontics and Pediatric Dentistry, School of Dentistry, University of Michigan, Ann Arbor, MI 48109
Juan Prieto
Department of Psychiatry, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
Hina Shah
Department of Psychiatry, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
Erika Benavides
Department of Periodontics & Oral Medicine, School of Dentistry, University of Michigan, Ann Arbor, MI 48109
Fabiana Soki
Department of Periodontics & Oral Medicine, School of Dentistry, University of Michigan, Ann Arbor, MI 48109
Yuji Mishina
Department of Biologic and Materials Sciences & Prosthodontics, School of Dentistry, University of Michigan, Ann Arbor, MI 48109
Margherita Fontana
Department of Cariology, Restorative Sciences and Endodontics, School of Dentistry, University of Michigan, Ann Arbor, MI 48109
Arvind Rao
Department of Radiation Oncology, University of Michigan, Ann Arbor, MI 48109
Department of Computational Medicine & Bioinformatics, School of Dentistry, University of Michigan, Ann Arbor, MI 48109
Hongtu Zhu
Department of Radiology and Biomedical Research Imaging Center, The University of North Carolina at Chapel Hill, Chapel Hill, NC 27599
Lucia Cevidanes
Department of Orthodontics and Pediatric Dentistry, School of Dentistry, University of Michigan, Ann Arbor, MI 48109