Breadcrumb
Periodontitis and Dementia Research
Association between Periodontal Disease and Cognitive Impairment in Adults
Periodontitis and Alzheimer’s Disease: Is There a Connection?
What is it?
Two review articles examining the connection between gum disease and neurodegenerative diseases, including Alzheimer’s, Parkinson’s and amyotrophic lateral sclerosis.
What problem does it aim to solve?
The global population is rapidly aging, with projections indicating that by 2030, the elderly population (≥65 years) will reach 1 billion, comprising 12% of the total global population, and by 2050, it will represent 16.7%. This demographic shift poses significant challenges, particularly concerning age-related diseases like dementia. Alzheimer’s disease, the most common form of dementia, is strongly associated with aging, with projections suggesting that by 2050, 1 in 85 individuals will be diagnosed with it. Notably, chronic periodontitis, primarily detected in older adults, affects over 50% of this population, highlighting the importance of understanding the link between periodontal inflammation and systemic complications.
How does it work?
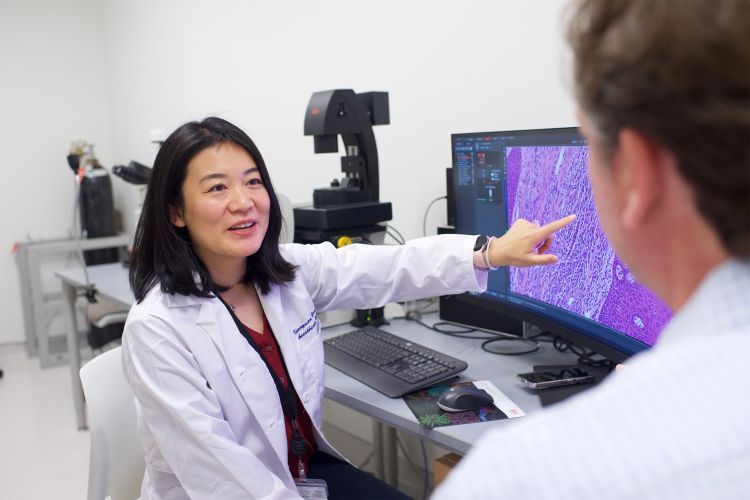
In the first review article, a comprehensive literature search was conducted to investigate the link between periodontitis and cognitive impairment. The review focused on studies examining the association between periodontal disease and dementia or neuroinflammation in adults. All quantitative studies were considered for inclusion, regardless of geographical location or assessment methods, while exclusion criteria comprised non-human studies, individuals under 18, and those with pre-existing neurological disorders.
A separate review examined the biology, evidence from human studies, evidence from animal studies, and therapeutic interventions to summarize the current understanding of the link between periodontitis and Alzheimer’s disease.
What are the real-world implications?
“Our mouth is the gateway to our body. This oral–systemic connection means that oral pathogens could lead to systemic diseases such as heart attacks, stroke, and Alzheimer’s disease. The finding of our systematic review came out confirming this connection … Taken as a whole, oral health should not be separated from the rest of body health; oral health must be prioritized in order to make serious steps toward better mental health.”
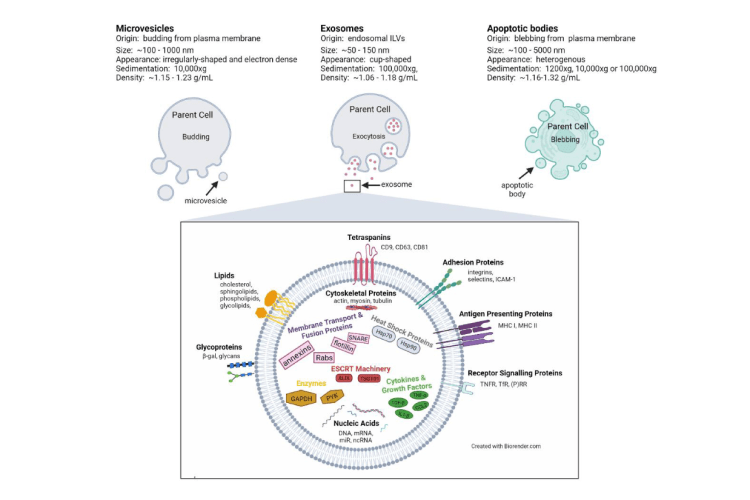
Looking at the bacteria in people's blood or the antibodies their immune system makes to fight these bacteria might help us predict who is at risk of getting Alzheimer’s disease when they're older.
What are the next steps?
More research to pinpoint the biological mechanism by which periodontitis can trigger the processes leading to dementia and neurodegenerative diseases.
Right now, we don't have strong proof that treating gum disease can affect how Alzheimer’s disease develops. In the meantime, it’s a good idea to focus on preventing gum disease in people who are at risk of getting Alzheimer’s disease (a worthy goal anyway). We also need to conduct more research to identify signs or biomarkers in the mouth that could tell us who is at risk for Alzheimer’s disease later in life.
Sources
“Association between Periodontal Disease and Cognitive Impairment in Adults”, Int. J. Environ. Res. Public Health 2023, 20(6), 4707
“Periodontitis and Alzheimer’s Disease: Is There a Connection?”, Oral 2024, 4, 61–73.
Authors
Najwane Said-Sadier
College of Health Sciences, Abu Dhabi University, Abu Dhabi 59911, United Arab Emirates
Batoul Sayegh
Neuroscience Research Center (NRC), Lebanese University, Beirut 1533, Lebanon
Raymond Farah
Neuroscience Research Center (NRC), Lebanese University, Beirut 1533, Lebanon
Linda Abou
Neuroscience Research Center (NRC), Lebanese University, Beirut 1533, Lebanon
INSPECT-LB (Institut National de Santé Publique, d’Épidémiologie Clinique et de Toxicologie-Liban), Beirut 1103, Lebanon
Rania Dweik
College of Health Sciences, Abu Dhabi University, Abu Dhabi 59911, United Arab Emirates
Norina Tang
Arthur Dugoni School of Dentistry, University of the Pacific, San Francisco, CA 94103, USA
Department of Periodontics, University of the Pacific, San Francisco, CA 94103, USA
Department of Laboratory Medicine, Veterans Affairs Medical Center, San Francisco, CA 94121, USA
David M. Ojcius
Dugoni School of Dentistry, University of the Pacific, San Francisco, CA 94103, USA
William Lundergan
Department of Periodontics, Arthur A. Dugoni School of Dentistry, University of the Pacific, San Francisco, CA 94103, USA
Kavitha Parthasarathy
Department of Periodontics, Arthur A. Dugoni School of Dentistry, University of the Pacific, San Francisco, CA 94103, USA
Navid Knight
Department of Periodontics, Arthur A. Dugoni School of Dentistry, University of the Pacific, San Francisco, CA 94103, USA